Table of Contents
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a terrifying event. It’s more than just feeling “shaken up” — PTSD causes long-lasting emotional distress, intrusive thoughts, and physical reactions that interfere with daily life.
Globally, around 5–10% of people will experience PTSD in their lifetime, with higher rates among survivors of war, abuse, accidents, or natural disasters. The good news is that with treatment and support, recovery is possible.
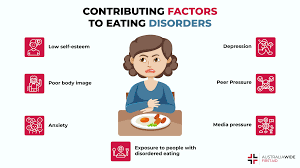
🔎 Causes / Risk Factors
PTSD develops after traumatic events such as:
- Violence or Abuse – Physical assault, sexual abuse, or domestic violence.
- Accidents & Injuries – Car crashes, natural disasters, or workplace accidents.
- War & Terrorism – Combat veterans, refugees, or survivors of bombings/attacks.
- Sudden Loss of Loved One – Death, suicide, or severe illness of a close person.
- Childhood Trauma – Neglect, bullying, or prolonged abuse.
Risk Factors That Increase PTSD Likelihood:
- Having a history of anxiety, depression, or mental illness.
- Lack of a support system (family/friends).
- Experiencing repeated or prolonged trauma.
- High-stress lifestyle with poor coping skills.
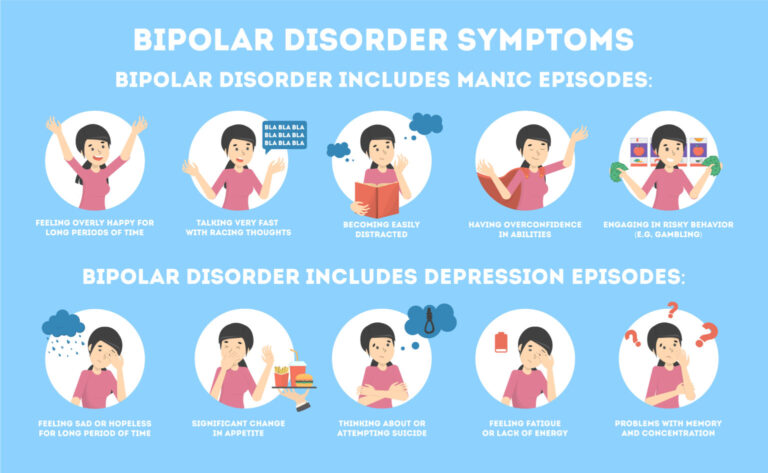
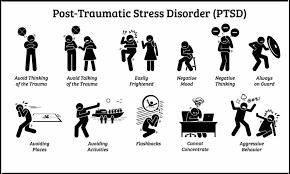
⚠ Common Issues / Symptoms
PTSD symptoms usually appear within 3 months of the trauma, but sometimes years later. They fall into four main categories:
🔴 Intrusive Memories
- Flashbacks — reliving the traumatic event.
- Nightmares or disturbing dreams.
- Severe emotional distress when reminded of the event.
🔵 Avoidance Symptoms
- Avoiding people, places, or conversations related to the trauma.
- Numbing emotions — feeling detached from others.
- Refusing to think or talk about the event.
⚡ Negative Changes in Mood/Thinking
- Hopelessness about the future.
- Memory problems, especially about the traumatic event.
- Difficulty maintaining relationships.
- Feelings of guilt, shame, or self-blame.
🔥 Physical & Emotional Reactions
- Hypervigilance (always “on edge”).
- Difficulty sleeping or concentrating.
- Irritability, angry outbursts, or aggressive behavior.
- Overreaction to sudden noises or touches.
📊 Table 1: Myths vs Facts
| Myths | Facts |
|---|---|
| PTSD happens only to soldiers | Anyone who experiences trauma can develop PTSD |
| People with PTSD are violent | Most people with PTSD are not violent; they struggle internally |
| PTSD is a sign of weakness | PTSD is a medical condition, not a weakness |
| Time heals all wounds | Untreated PTSD can last for years or worsen |
| Talking about trauma makes PTSD worse | Talking through therapy helps healing |
📋 Table 2: Do’s and Don’ts
| Do’s ✅ | Don’ts ❌ |
|---|---|
| Seek professional help (psychiatrist/therapist) | Hide or suppress traumatic memories |
| Build a strong support network | Isolate yourself completely |
| Practice grounding techniques (breathing, mindfulness) | Use alcohol/drugs to cope |
| Maintain a healthy routine (exercise, sleep, nutrition) | Stay in denial or ignore symptoms |
| Be patient — recovery takes time | Expect overnight recovery |
🌱 Prevention / Awareness Tips
- Early Intervention: Seek counseling immediately after traumatic events.
- Peer & Family Support: Talking about experiences reduces isolation.
- Stress-Relief Practices: Yoga, meditation, journaling, or art therapy.
- Awareness Campaigns: Reduce stigma around mental health and trauma.
- Self-Care Habits: Balanced sleep, exercise, and limiting caffeine/alcohol.
- Emergency Helplines: Know available hotlines in case of crisis.
💊 Treatment / Care
PTSD is treatable with the right approach:
- Psychotherapy (Talk Therapy):
- Cognitive Behavioral Therapy (CBT): Helps reframe negative thoughts.
- Exposure Therapy: Gradual exposure to trauma reminders in a safe way.
- EMDR (Eye Movement Desensitization & Reprocessing): Reduces distress linked to memories.
- Medications:
- Antidepressants (SSRIs, SNRIs) for mood regulation.
- Anti-anxiety drugs for short-term relief.
- Sleep aids in severe insomnia (under doctor’s advice).
- Lifestyle Approaches:
- Exercise, healthy diet, social interaction, mindfulness.
- Avoid alcohol or recreational drugs.
⚡ Recovery may take months or years, but support + treatment = healing.
📖 Case Study / Real-Life Example
After the 2004 Indian Ocean tsunami, many survivors developed PTSD. Relief agencies introduced community counseling, art therapy, and group healing circles. Within a year, studies showed a significant drop in PTSD symptoms among participants compared to those who avoided therapy.
This highlights that timely counseling and support can prevent long-term suffering.
❓ FAQs
Q1. Can PTSD go away on its own?
A1. Sometimes mild cases improve, but most require therapy and support.
Q2. Is PTSD permanent?
A2. Not necessarily. With treatment, symptoms can be managed or eliminated.
Q3. How is PTSD different from normal stress?
A3. PTSD symptoms are severe, long-lasting, and disrupt daily life.
Q4. Can children develop PTSD?
A4. Yes. Children exposed to abuse, violence, or disasters can develop PTSD.
Q5. Is medication the only solution?
A5. No. Best results come from therapy + lifestyle + sometimes medication.
Q6. Can PTSD be prevented?
A6. Early counseling and strong support systems after trauma reduce the risk.
🏁 Conclusion
PTSD is a serious but treatable condition that can affect anyone who has experienced trauma. Awareness, empathy, and early help are key in breaking its grip.
💡 Remember: Healing from trauma takes time — but it is always possible with the right support and treatment.